Overview
Cityblock Health is a tech-enabled provider of health care and social services to low-income and racially diverse populations.
Strategic goals
Cityblock implemented its virtually integrated care model to:
- Ensure continuity of complex care management for a diverse, older patient population during a pandemic.
- Maintain or lower cost of care for members by reducing avoidable emergency department visits and inpatient admissions.
Program impact on health care value streams
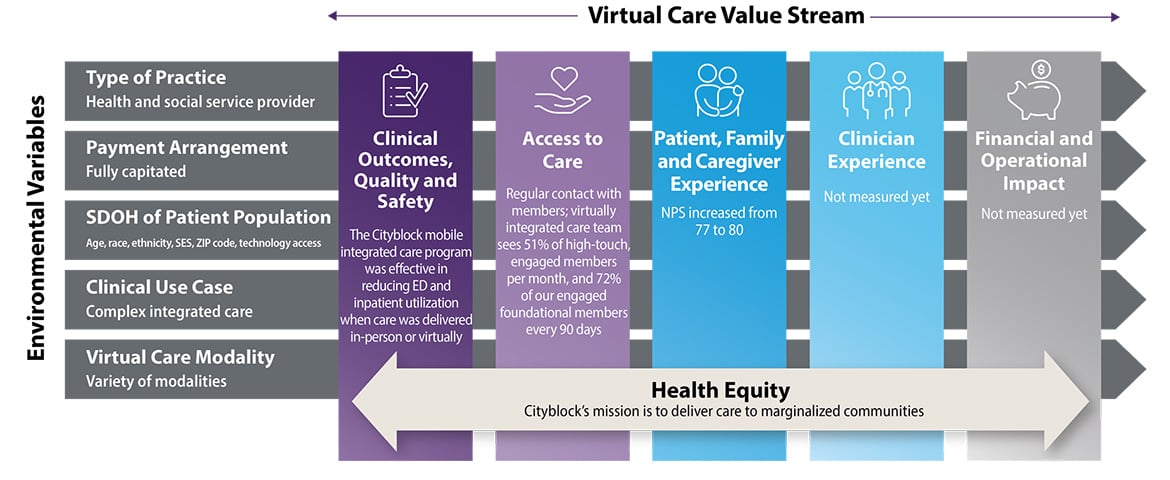
Founded in 2017, Cityblock contracts with payers to provide primary care, behavioral health care and social services to members with complex needs. One of Cityblock’s unique virtual care models adopted during the COVID-19 pandemic, the mobile integrated care program, leverages a variety of modalities (including interprofessional consult, video and phone visits, SMS messaging, and in-home care) to deliver whole-person, complex care management to marginalized communities in New York, Massachusetts and Connecticut.
Over half of the members who receive services through this model are over 60 years old, and more than half (59%) are women. Approximately 25% of members receiving services through the model identify their race or ethnicity as Black, 21% are white, 3% are Hispanic, 7% are multiracial, and 32% did not identify their race or ethnicity.
Payers provide Cityblock an annual capitated payment for each member, and if Cityblock is able to manage its total membership’s care for lower cost than projected, it keeps those savings. Cityblock assumes financial responsibility for medical expenses beyond the capitated payment rate.
At the onset of the COVID-19 pandemic, Cityblock recognized the need to adapt its traditional care model and workflow to engage patients virtually to prevent disease spread and continue delivering care management to patients in the safety of their homes. To address this need, Cityblock developed and began implementing the mobile integrated care program for a subset of Cityblock members.
In the early stages of this virtual approach, Cityblock sent members links to participate in video appointments; however, many members faced connectivity challenges, which resulted in high no-show rates. To address these barriers, Cityblock launched a pilot where they delivered computer tablets directly to members’ homes.
The pilot quickly showed that tablets alone weren’t sufficient to increase successful connection rates, as the tablet software proved to not be designed to meet the needs of many of their older members who require additional support to successfully connect with Cityblock clinicians. Cityblock ultimately achieved success in its virtual approach when it deployed emergency medical technician (EMT) teams with telehealth technology to members’ homes, with the EMT acting as an in-home extender to the telehealth clinician. This hands-on approach helped bridge gaps in upfront solution design that had limited access for certain members, resulting in successful video visits between members and their Cityblock care team.
Cityblock’s virtually integrated care team is comprised of a community health partner (with a similar background and training as a community health worker), nurse care manager, nurse practitioner or physician primary care provider, behavioral health therapist and psychiatrist. The community health partner is responsible for checking in with the member via phone or text on an ongoing basis to understand their care plan progress and flag issues for the rest of the medical team as necessary.
Members generally meet with a therapist for behavioral health support once a week via video visit. Medical visits are also delivered in a virtual manner, wherein a clinician connects to the member via video visit and the EMT is at the patient’s home to help initiate the video visit, collect vitals, collect labs and conduct a physical exam, as appropriate.
Clinical outcomes, quality and safety
The Cityblock mobile integrated care program was similarly effective in reducing ED and inpatient utilization regardless of whether it was delivered in-person or virtually.
Access to care
Regular contact with membership: Regular contact with members; virtually integrated care team sees 51% of high-touch, engaged members per month, and 72% of our engaged foundational members every 90 days.
Patient, family and caregiver experience
Net Promoter Score: NPS increased from 77 to 80.
Cityblock’s mission is to “deliver personalized health services to marginalized communities [and] reduce disparities and rebuild trust between health care providers, social services organizations, and marginalized groups.”
Source: Data and content for this case study was provided by and used with permission from Cityblock Health.
Download the case study (PDF) and read other Return on Health telehealth case studies and scenarios.