As physicians advance through their careers in medicine, from the rigorous demands of residency to the relentless pressure of long-term practice, a pattern has emerged. The number of years a physician has been in practice may be a telling indicator of burnout risk, according to an exclusive survey from the AMA.
As the leader in physician well-being, the AMA is reducing physician burnout by removing administrative burdens and providing real-world solutions to help doctors rediscover the Joy in Medicine™.
More than 12,400 responses from physicians across 31 states were received from 81 health systems and organizations who participated in the AMA Organizational Biopsy® last year. The AMA national physician comparison report—which is exclusive data to the AMA that is not published anywhere else—reflects 2023 trends in six key performance indicators: job satisfaction, job stress, burnout, intent to leave an organization, feeling valued by an organization and total hours spent per week on work-related activities (known as “time spend”).
The purpose of the aggregated data is to provide a national summary of organizational well-being and to serve as a comparison for other health care organizations. The results may be limited by the health systems that chose to participate.
In 2022, 61% of physicians who were six to 10 years postresidency or fellowship training reported at least one symptom of burnout, compared with 54% of doctors who were one to five years out from training.
For 2023, here is what AMA data reveals about physician burnout rates and how they vary based on the number of years since completing residency or fellowship training:
- 1–5 years: 46.7%—down from 54%.
- 6–10 years: 55.1%—down from 61%.
- 11–15 years: 55.3%—down from 59%.
- 16–20 years: 50.8%—down from 56%.
- 20 or more years: 41.3%—down from 46%.
Meanwhile, job satisfaction was highest in early and late-career physicians. For physicians who were five or fewer years out of training, 74.7% reported they were satisfied with their jobs. And for physicians with 20-plus years since residency or fellowship, 72.9% reported job satisfaction. But job satisfaction rates were lowest for physicians with 11 to 15 years in practice, at 69.2%.
Additionally, 45.2% of physicians six to 10 years post training felt valued by their organization compared with 54.6% who are 20-plus years in practice.
At Ochsner Health, 75.1% of physicians reported feeling satisfied with their jobs, up from 73.2% in 2022. Ochsner Health is a member of the AMA Health System Program, which provides enterprise solutions to equip leadership, physicians and care teams with resources to help drive the future of medicine.
Here is how Ochsner Health is taking steps to reduce physician burnout and improve job satisfaction among all years in practice.
Translating the data to burnout help
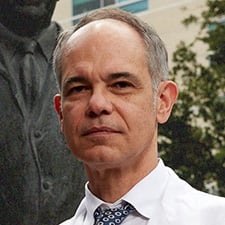
Nigel Girgrah, MD, PhD, chief wellness officer and medical director of liver transplantation for Ochsner Medical Center in New Orleans, said data collected by Ochsner echoes what the AMA survey found, specifically related to years in practice.
“We know that our physicians who have been in practice for between 10 and 15 years seem to be the most burnt out—50.3% compared to overall as an organization, 44%,” Dr. Girgrah said. “We can speculate why that might be. … Their practice is more mature, so they're at their busiest. You could also speculate that this is when they're starting families or the kids are becoming a little bit more of a handful, or they've got more family responsibilities, both with kids and older, aging parents.”
In response, Ochsner Health has expanded both child care and elder care services, and significantly improving paid parental leave policies. Now, all full-time employees, including physicians, are eligible on the first day of their employment for parental leave at 100% of their base pay for six weeks upon the addition to their household of a child by birth, adoption or surrogacy.
Ochsner also recently changed a policy that used to rescind senior-physician status to those who dropped their hours to part-time.
“We've been doing a lot around efforts to reduce, in general, distress in the workplace,” Dr. Girgrah said.
Using AI to tackle documentation woes
Ochsner Health also uses augmented intelligence (AI)—often called artificial intelligence—to help. Through a pilot program across its 46-hospital system, Ochsner Health uses generative AI listening tools to help reduce the administrative burden on physicians.
In the program, physicians use ambient AI to listen while they converse more freely with patients during encounters and help produce clinical notes in the EHR for the physician to review, approve and sign. AI can also provide help for physicians responding to inbox messages.
“Generative AI will actually propose a response to a message,” Dr. Girgrah said, in which it can “mine the charts” and offer an answer. Physicians approve and sign off on all communication and health records, but the reduction in time spent in the EHR, known to be a driver of burnout, can help free up valuable time both in and out of the office.
“The early data has been incredibly positive in terms of those who have gone through the pilot,” Dr. Girgrah said.
One quote from a physician in orthopedics demonstrated the success. The physician said, “It’s 2 p.m. in a busy clinic, and all my notes are done.” Patients have also reported being happy with how engaged their physicians are in their care.
There is a “commitment to scale very quickly” the pilot program across the health system, said Dr. Girgrah.
Tailoring programs to the need
Ochsner has done its own measuring of the scope of burnout in its health system, Dr. Girgrah said, determining when and where the problem may be most severe. That helps target the use of limited resources. For example, he said, the organization offers one-on-one coaching.
“With this data from the Organizational Biopsy, we can offer that with a little more specificity, knowing that we can't offer every physician one-on-one coaching,” he said. “But we know where to look in terms of who may need it the most.”
Another example is a leadership retreat offered by Ochsner in which they take physicians and senior administrative leaders offsite for three days to take a "deep dive into understanding themselves" and into what makes them happy, said Dr. Girgrah.
While there isn’t a “cause and effect” improvement on burnout statistics, “there is a correlation,” he said, noting that overall, burnout in the health system is 44.4%, but for those who have gone through the leadership program, it’s 26.5%.
Data helps in “recognizing that we have limited bandwidth in terms of what we can offer, but knowing who to go to first and which demographic areas within our physician group practice has the greatest need,” Dr. Girgrah said.