Evidence indicates that shift-to-shift handoffs are related to increases in adverse events and patient mortality. And a new study examines the link between death risk and end-of-rotation transitions, but what kinds of strategies can work in practice to minimize the handoff hazard?
A study published in the recent Journal of the American Medical Association (JAMA) theme issue on medical education asks the question, “Are patients who are exposed to end-of-rotation resident transition in care at risk for greater mortality?”
Examining more than 230,000 patients admitted to internal medicine services in 10 Veterans Affairs (VA) hospitals, the study found that end-of-rotation house staff transition in care was associated with significantly higher in-hospital mortality when handoffs involved only interns, or interns and residents. But they the death rate was not higher when transitions involved only residents. The higher death risk “may be limited to longer-stay, complex patients with greater comorbidities or those discharged soon after the transition,” the authors concluded.
In an editorial, “Inpatient Service Change: Safety or Selection?” Vineet M. Arora, MD, pointed out that “patients who remain hospitalized during a change in personnel on the inpatient service are likely different than those who are discharged. This selection helps to explain the increased mortality with service changes reported in the study.”
“Given well-documented content omissions during handoffs, it is plausible that poor information exchange during service change contributed to increased in-hospital mortality,” wrote Dr. Arora, director of graduate medical education (GME) clinical learning environment innovation at the University of Chicago.
But, she wrote, there are alternative explanations. For example, a patient admitted before transition may receive less attention from the team that admitted them since they will not continue that patient’s care throughout their hospital stay. Or the team taking over “may perceive they never really ‘owned’ a patient they did not admit.”
“In contrast, an intern-resident service change could facilitate a ‘fresh look’ at an ill patient who may not benefit from ongoing intervention,” Dr. Arora said.
The findings yet again draw attention to the critical importance of improving in-hospital care transitions.
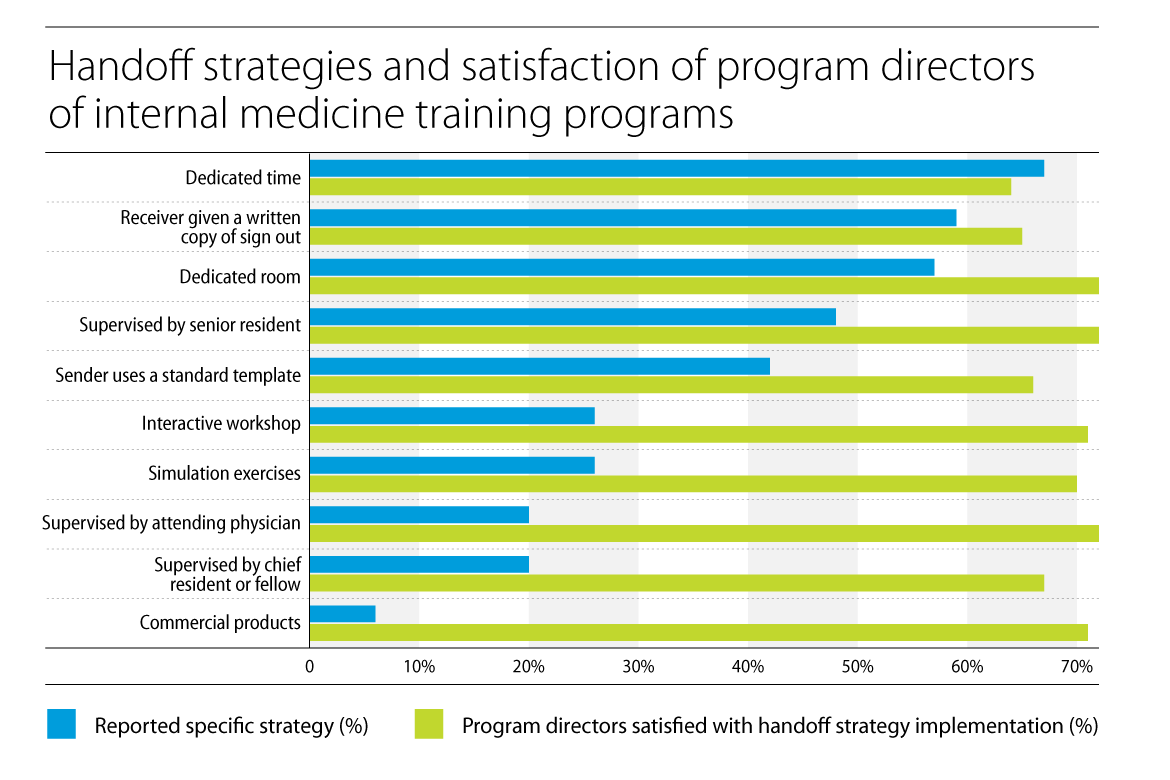
Dr. Arora also helped conceive and design a survey whose results were included in the JAMA medical education theme issue. The survey which asked residency programs which techniques they were using in practice to make handoffs smoother and safer for patients. These included educational resources, carving out dedicated time for handoffs and adding supervisors to transitions, among others (below).
Dr. Arora works closely with residents every day. When asked about some of the ways she’s found to make transitions in care at end-of-rotation easier for residents, she offered three examples:
- Standardizing templates to help with transfer of content: This is “especially important since service changes often require more information about disposition and discharge planning than a traditional shift handoff,” Dr. Arora said.
- Structuring handoffs so there is enhanced continuity of team members: “Instead of everyone changing at once,” she said, “either the resident or attending stays on the team a bit longer so there is someone on the team who knows the patient.”
- Encouraging the patient and their family to be more involved: “Studies suggest they often don’t know a handoff has occurred,” Dr. Arora said. “We have piloted bedside handoffs at service change for select patients to see if that could help [and] the pilot was demonstrated to be feasible in our hospitalist program. One challenge is structuring a shift or protecting time for hospitalists to do it, [which] may be harder to do in a resident program but it’s worth considering ways to empower patients and caregivers in this way.”
“It is reasonable to suggest that service changes may be risky for patients and to explore ways to improve them,” Dr. Arora said. “Until further research elucidates the reasons why mortality may increase at these times, academic health centers must remain committed to ensure the safety of patients at all times, especially those patients undergoing service changes.”