A recent federal bill is seeking to authorize grants for graduate medical education (GME) positions in states that have a low rate of medical residents relative to the general population, increasing residency slots in needed areas.
 The Creating Access to Residency Education Act of 2014, also known as the CARE Act, “offers a creative solution” to ensuring access to care and expanding the physician workforce, AMA Executive Vice President and CEO James L. Madara, MD, said in a letter to the bill’s sponsors, U.S. Reps. Kathy Castor, D-Florida, and Joe Heck, R-Nevada.
The Creating Access to Residency Education Act of 2014, also known as the CARE Act, “offers a creative solution” to ensuring access to care and expanding the physician workforce, AMA Executive Vice President and CEO James L. Madara, MD, said in a letter to the bill’s sponsors, U.S. Reps. Kathy Castor, D-Florida, and Joe Heck, R-Nevada.
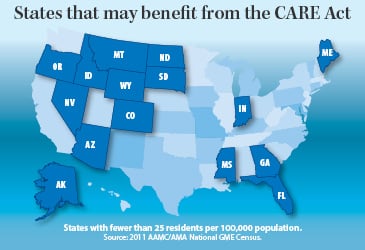
If passed, the bill would create a $25 million grant program through the Centers for Medicare & Medicaid Services that would allow certain hospitals to apply for matching funds to support new medical residency training positions. Only public or nonprofit teaching hospitals or accredited GME training programs in a state with fewer than 25 medical residents per 100,000 people would be eligible for funding.
The grant recipient must cover one-third of the cost for new primary care residency positions and one-half of the costs for any other field. However, the bill encourages such organizations to enter into partnerships with states, local governments, community health centers, local health departments and other appropriate organizations to cover the remainder of the expense.
Expanded insurance coverage under the Affordable Care Act is expected to increase demand for primary care physicians by 14 percent by 2025, according to a recent report from the AMA Council on Medical Education. More insured patients, combined with an aging population and retiring physicians, will contribute to the need for more physicians to enter the workforce.
Medical schools have increased their class sizes to help meet this need, but a proportional increase of GME positions has yet to happen, the report noted. Medicare’s current cap on financial support for GME prevents teaching hospitals from increasing the number of residency training positions and often prevents new hospitals from establishing teaching programs. The AMA has been calling for increased federal funding for GME positions via its SaveGME campaign and has been advocating for new or expanded residency programs in rural and other underserved locations.
The CARE Act’s focus on areas with significant need would mean 16 states—including Mississippi, Wyoming, Idaho and Florida—would be eligible for funding, all of which have fewer than 25 medical residents per 100,000 people, according to a 2013 report from the Association of American Medical Colleges.
As part of its Accelerating Change in Medical Education initiative, the AMA is working with 11 medical schools from across the country to establish innovative new medical education models. Emphasis on primary care and programs that address the unique needs of underserved populations is a core factor of several programs. Students graduating from Brown University Warren Alpert Medical School’s new program, for instance, will hold a dual degree, MD-ScM, in population medicine with training in health disparities and social determinants of health.