The United States Medical Licensing Examination® (USMLE®) Step 1 exam is often the first major test of a medical student’s knowledge, and some of its questions are missed by all but a select few highly prepared test takers. Check out this month’s question that Kaplan Medical says stumps most students, and view an expert video explanation of the answer. See all posts in this series.
Think you have what it takes to rise above your peers? Test your USMLE knowledge below.
Ready. Set. Go.
This month’s question that stumped most students
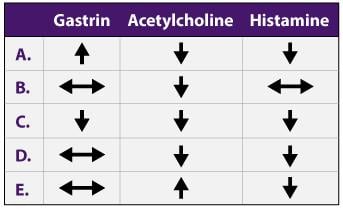
Gastrin, acetylcholine and histamine all regulate gastric acid secretion from parietal cells under normal conditions. Administration of atropine will most likely cause which of the following changes in the ability of gastrin, acetylcholine and histamine to stimulate acid secretion?
The correct answer is C.
Kaplan Medical explains why
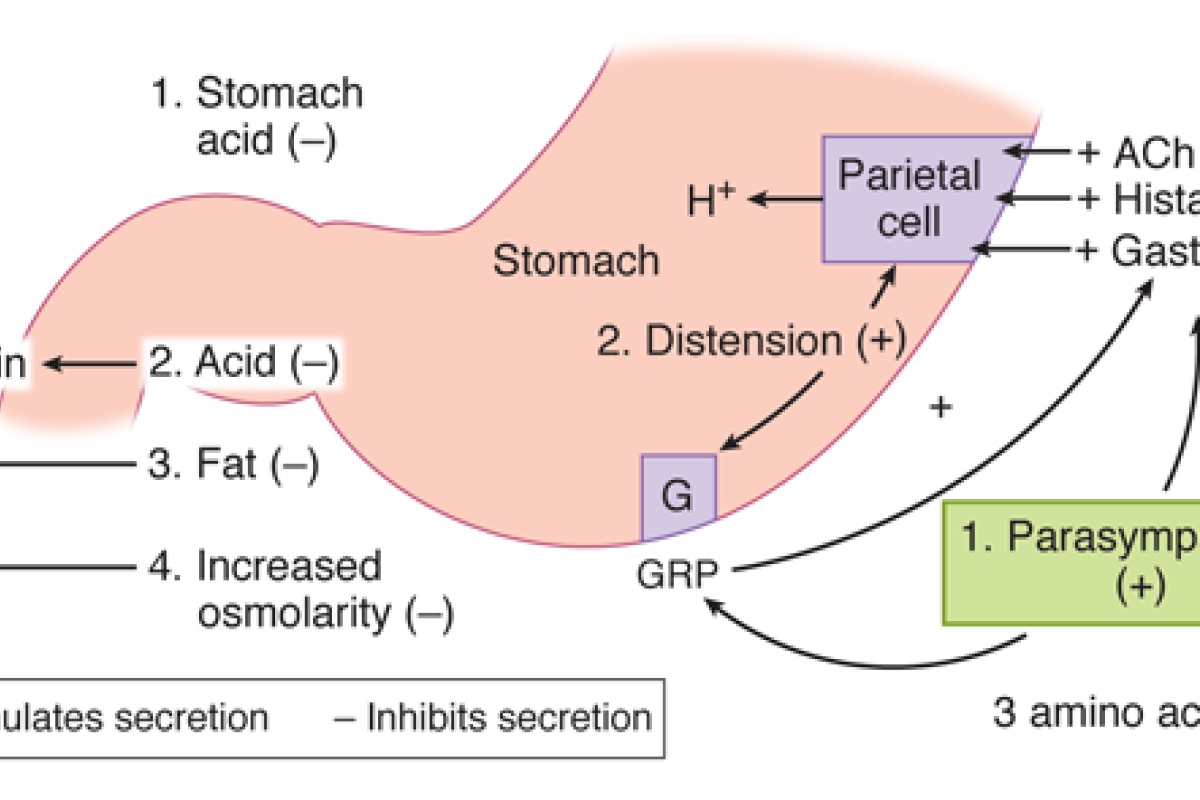
Parietal cells express at least five different receptors types that control acid secretion—three excitatory, two inhibitory. All five receptors signal their occupancy via G-proteins. The three excitatory receptors bind acetylcholine (ACh), gastrin and histamine.
- The ACh receptor is an M3 AChR that activates in response to ACh released from vagal nerve endings. It couples intracellularly via Gq to the IP3 signaling pathway. The AChR facilitates reflex acid secretion in response to the sight and smell of food (a vagovagal reflex).
- Gastrin binds to a cholecystokinin B (CCKB) receptor that also couples intracellularly via Gq to the IP3 signaling pathway. Gastrin is released from G cells located in the gastric mucosa. They release gastrin in response to luminal peptides and amino acids whose appearance indicates that a meal has begun. G-cells are also regulated by the vagus nerve, but the nerve terminals signal via a peptide neurotransmitter (gastrin releasing peptide; GRP) rather than the usual ACh.
- Histamine binds to an H2 receptor that couples via Gs to the cAMP intracellular signaling pathway. Histamine originates from enterochromaffin-like (ECL) cells, which are neuroendocrine cells located in the gastric mucosa. ECL cells secrete histamine when stimulated either by the autonomic nervous system or by gastrin.
- ECL cells are innervated by the vagus nerve. They are activated via ACh release and an M3 AChR.
- ECL cells also express CCKB receptors, which allows them to respond to gastrin when G cells are activate.
Histamine is the primary stimulus for gastric acid secretion. Even though ACh and gastrin are secretagogues also, their effects are entirely secondary to histamine. Thus, mice models lacking H2 receptors are unable to secrete acid, even when the vagus nerve and G-cells are active and releasing ACh and gastrin, respectively. The importance of the histamine pathway is also reflected in the efficacy of H2 blockers (e.g. cimetidine, ranitidine) in controlling acid secretion in patients with peptic ulcers and gastroesophageal reflux disease. Note that H2 blockers, unlike knock-out studies, cannot inhibit the histamine pathway by 100%. Any residual H2 receptor signaling is subsequently potentiated by the ACh and gastrin pathways, which is why proton pump inhibitors (e.g. omeprazole) have replaced H2 blockers as the drugs of choice in controlling gastric acid production.
Under normal circumstances, all three secretagogues are released during a meal and all three receptor types are active and their effects on acid secretion are multiplicative; their combined actions are greater than might be expected from the sum of their individual actions. This phenomenon is known as “potentiation”, and reflects the power of G-protein signaling pathways to interact with and amplify sensory signals.
Atropine is an M-type AChR (mAChR) antagonist. Referring to the pathways above, it would be expected to block the parietal cell mAChR and the mAChR on ECL cells. The ability of ACh to stimulate acid secretion is, thus, clearly reduced.
Because gastrin and histamine act through different receptor types that are not blocked by atropine, their ability to stimulate acid secretion might be expected to be resistant to mAChR blockade. In practice, however, the phenomenon of potentiation means that the loss of the ACh-mediated signal decreases the potency of both gastrin and histamine, so all three secretagogues have decreased efficacy when atropine is applied (choice C).