The Medicare Economic Index (MEI) is a measure of practice cost inflation that was developed in 1975 to estimate annual changes in physicians’ operating costs and establish appropriate Medicare physician payment updates.
Background
Although the 1972 legislation mandating its creation did not specify the type of index to be used, the MEI’s general form followed recommendations made by Congress. It consists of two categories reflecting the resources used in medical practices: (1) physician practice costs and (2) physician compensation (physician work).
The physician practice costs portion of the current MEI includes components for nonphysician compensation (including fringe benefits), medical supplies, professional liability insurance and other expenses (including other professional services). Each component is assigned a weight and various proxy indices are used to estimate price changes.
The physician compensation category of the MEI reflects increases in general earnings and is currently proxied by changes in the wages and benefits of professional occupations in the U.S. from the Bureau of Labor Statistics. The change in the combined practice costs and physician compensation components of the MEI is then adjusted (reduced) by the 10-year average of economy-wide multi-factor productivity.
Diminishing role of the MEI
When the Medicare Fee Schedule (MFS) was established in 1992, the role of the MEI in determining annual physician payment updates was diminished considerably. Annual payment updates were based on the MEI, but were further adjusted according to whether aggregate Medicare physician spending fell below or exceeded a prospectively-established expenditure target; first by the Medicare Volume Performance Standards (MVPS) and later by the Sustainable Growth Rate (SGR). Under the expenditure targets, physician payments were cut across-the-board to offset aggregate spending increases that exceeded the target in a given year, or they could be increased across-the-board when aggregate spending fell short of the target.
For many reasons, the expenditure target systems were fatally flawed. They did keep rates of growth in overall Medicare physician spending low, but the targets quickly produced payment cuts that were unsustainable. The problem was amplified by Congressional actions that stopped the most severe cuts for only a year (or a few months) at a time by subtracting the cost of these payment “patches” from projected updates later in the budget window. By 2015, physicians were facing a payment cut of 21%.
The Medicare Access and CHIP Reauthorization act (MACRA) of 2015 made significant changes to the payment system. Most notably, it eliminated the SGR and the “debt” that had accumulated over more than a decade of annual payment patches. However, one flaw immediately became apparent. The MEI no longer played any role in annual payment updates. Instead, for budgetary reasons, MACRA’s updates were set by statute at numbers that from the beginning were judged unsustainable. Those updates, all of which fall well below any measure of inflation, were set at:
- 0.5% for 2016–2019
- 0.25% in 2026 onward for traditional fee-for-service
- 0% for 2020–2025
- 0.75% in 2026 onward for advanced alternative payment models
It is widely recognized that chronically inadequate Medicare payment rates will have an impact on access to care. This was recognized again recently by the Medicare Trustees, who noted in their 2023 Medicare Trustees Report:
“While the physician payment system put in place by MACRA avoided the significant short-range physician payment issues resulting from the SGR system approach, it nevertheless raises important long-range concerns that will almost certainly need to be addressed by future legislation…. [T]he law specifies the physician payment updates for all years in the future, and these updates do not vary based on underlying economic conditions, nor are they expected to keep pace with the average rate of physician cost increases. The specified rate updates could be an issue in years when levels of inflation are high and would be problematic when the cumulative gap between the price updates and physician costs becomes large. Absent a change in the delivery system or level of update by subsequent legislation, the Trustees expect access to Medicare-participating physicians to become a significant issue in the long term.”
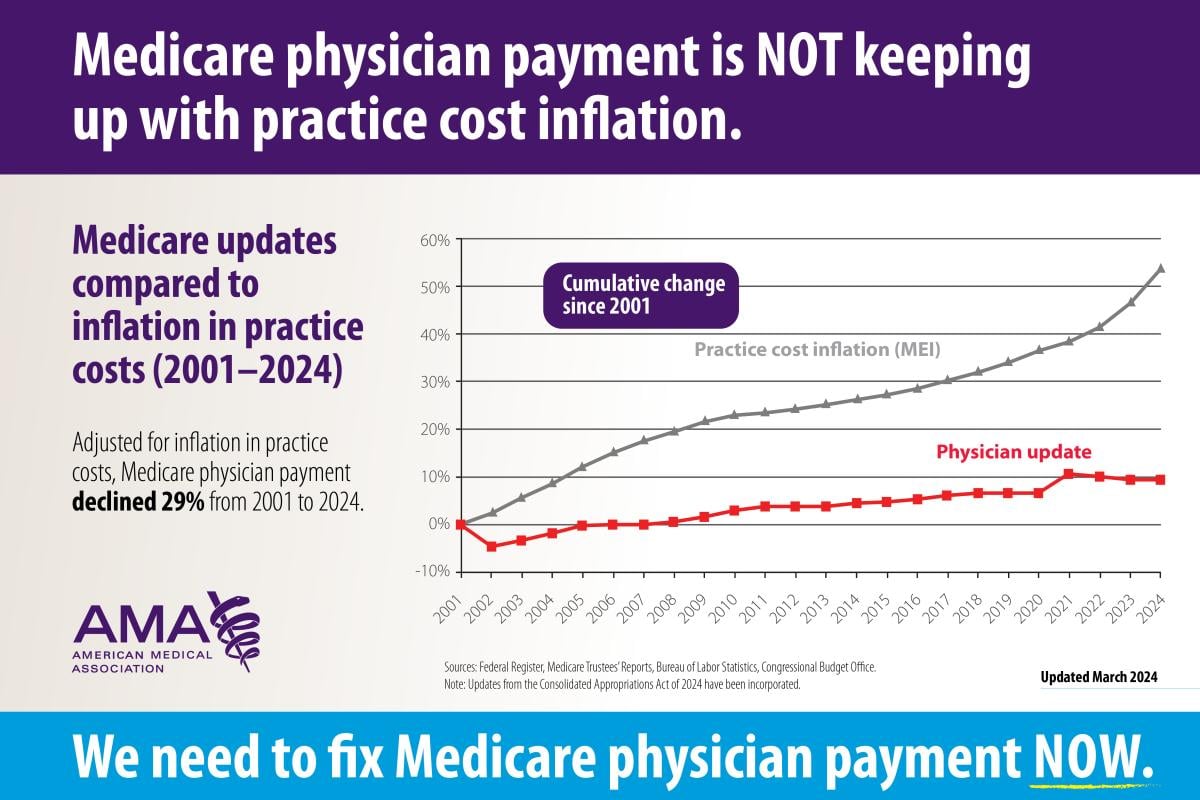
As shown below, the problematic cumulative gap between MFS updates and physician costs has grown quite large. From 2001 to 2024, Medicare physician payment has declined 29% when adjusted for inflation in practice costs.
Legislative solutions
Physicians in all specialties and across the country agree that the current Medicare physician payment system needs reform, and that an annual inflationary update must be the foundation of any reforms. Providing an MEI update for physician payments like those provided to virtually all other Medicare providers will enable physician practices to better absorb other payment redistributions triggered by budget neutrality rules and performance adjustments, as well as periods of high inflation and rising staffing costs. It will also help physicians invest in their practices and implement new strategies to provide high-value care.
Learn more about Medicare basics
The AMA's Medicare Basics series provides an in-depth look at important elements of the Medicare physician payment system. Find more topics about the payment system and why it's in need of reform.
Additional AMA resources on Medicare payment reform
- FixMedicareNow.org
- AMA fights against Medicare cuts, defending practices & access to care
- Current Medicare payment system on unsustainable path: Contact Congress
- Principles for Medicare physician payment reform
- Advocacy in action: Leading the charge to reform Medicare pay
- AMA advocacy efforts
- AMA leads on Medicare reform