Extracorporeal membrane oxygenation (ECMO) is giving a new lease on life to patients with life threatening heart and lung failure at University of Iowa (UI) Health Care.
The hospital excels at the cardiovascular life-support technique, achieving national and international recognition in use of the process. Known as a pediatric trauma center, UI is one of the few academic ECMO centers in the U.S. that supports adult, pediatric and neonatal populations.
It's important to distinguish ECMO as a supportive lifesaving therapy, not itself a treatment, said Lovkesh Arora, MD, an anesthesiologist and critical care intensivist with University of Iowa Health Care, which is a member of the AMA Health System Program that provides enterprise solutions to equip leadership, physicians and care teams with resources to help drive the future of medicine.
The goal of ECMO, Dr. Arora said, is to allow the heart and lungs to rest and recover while providing adequate circulatory support and oxygenation to vital organs.
The Extracorporeal Life Support Organization (ELSO) classifies UI’s program as a platinum-level center of excellence. “There are nearly 800 ECMO centers in the world, 43 of those 800 have platinum level status and we are proud to be one of them,” Dr. Arora noted.
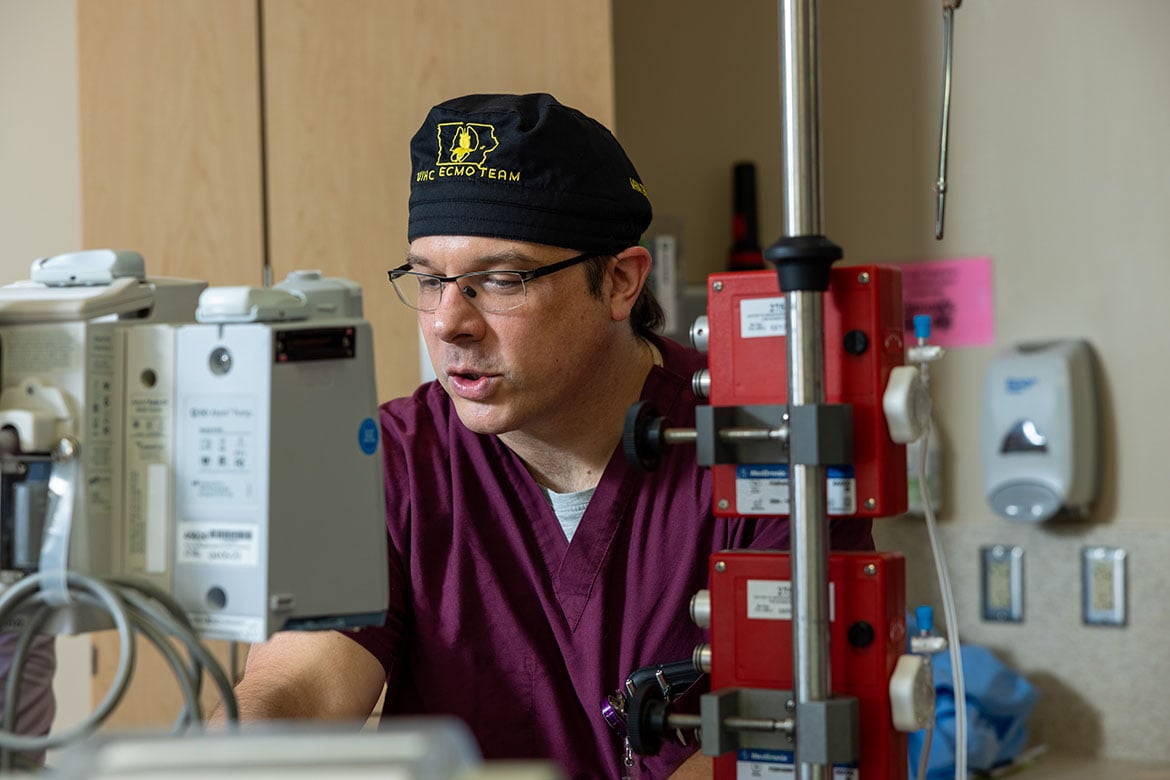
How ECMO works
The ECMO team is truly multidisciplinary, consisting of critical care physicians, surgeons, nurses, respiratory therapists and physical therapists. "It needs the whole team to make this endeavor of taking care of ECMO patients successful,” said Dr. Arora.
When patients develop acute heart or lung failure, they are typically able to be supported with conventional measures such as medications and ventilators. It is when those conventional measures fail, ECMO can be used to allow patients more time to recover.
There are two major ECMO supportive therapies. Veno-venous ECMO (V-V ECMO), mainly supports the lungs, and veno-arterial ECMO (VA-ECMO) supports both heart and lungs.
“The whole idea of ECMO therapy is to give adequate rest to the heart and lungs, come up with intervention strategies to make them better, but at the same time support rest of the vital organs, which still need the blood supply, and the oxygen” Dr. Arora said.
The procedure isn’t for everyone. ECMO requires anticoagulation, so a common complication is bleeding. This makes the therapy complex, for example: “Trauma patients often have life threatening heart and lung failure but due to severe bleeding, ECMO may not be able to be utilized,” he explained.
Numbers show flourishing program
ECMO programs are growing: More than 100 new ECMO programs started up in the U.S. in the last 3-5 years. There are about 300 to 400 U.S. ECMO programs, including the UI’s.
“We do around 60 to 70 ECMOs in a year,” supporting all kinds of populations, said Dr. Arora. About 40 to 45 ECMOs take place in adults, 20 to 25 are in children and neonates.
Survival in VV-ECMO averages 60–63%, and 40–42% for VA-ECMO. Outcomes are poorer in the latter category because these patients are often sicker.
“Our hospital to discharge survival rates match other major academic medical centers,” said Dr. Arora.
Pairing ECMO with physical therapy
UI also has a dedicated physical therapy team that makes a range of motion exercises possible for ECMO patients.
The team ambulates ECMO patients with cannulas in the groin or in the neck.
“Our goal for the patients is to dangle their feet, to maybe stand up, and maybe walk by day three or day four after they get on ECMO,” said Dr. Arora.
Just putting a patient on ECMO is not the end of the story, he stressed. “We still have to do all those things that can make other organs healthier.”
ECMO treatment is an extra stressful event added to the physical, mental, and other stresses inherent in patients who require ICU admission. The mental well-being of the patient is very important, too. “It’s not easy to ambulate ECMO patients with big cannulas in the groin, but with the right kind of people, we move them around, we walk them around, we take them out in the fresh air.”
Building on ECMO achievements
In future projects, UI is hoping that Extracorporeal Life Support Organization will endorse its educational course in ECMO. The goal is to make UI’s program a regional educational hub in the Midwest for all specialists using ECMO, said Dr. Arora.
University of Iowa Health care also plans to roll out a new procedure called extracorporeal cardiopulmonary resuscitation (eCPR), a process that emergently applies ECMO to cardiac arrest patients who don’t respond to conventional CPR.
eCPR’s success depends on early transfer of eligible patients to the cardiac catheterization laboratory, quick initiation of ECMO, and collaboration among multidisciplinary teams, said Dr. Arora.