Physicians urge MedPAC to recommend inflation-based Medicare payment update to replace current law
In a letter (PDF) to the Medicare Payment Advisory Commission (MedPAC), the AMA expressed support for the direction of the Commission’s deliberations at the April 2024 meeting to replace the severely inadequate baseline physician payment updates in current law with an annual update that accounts for inflation in the costs of running a medical practice.
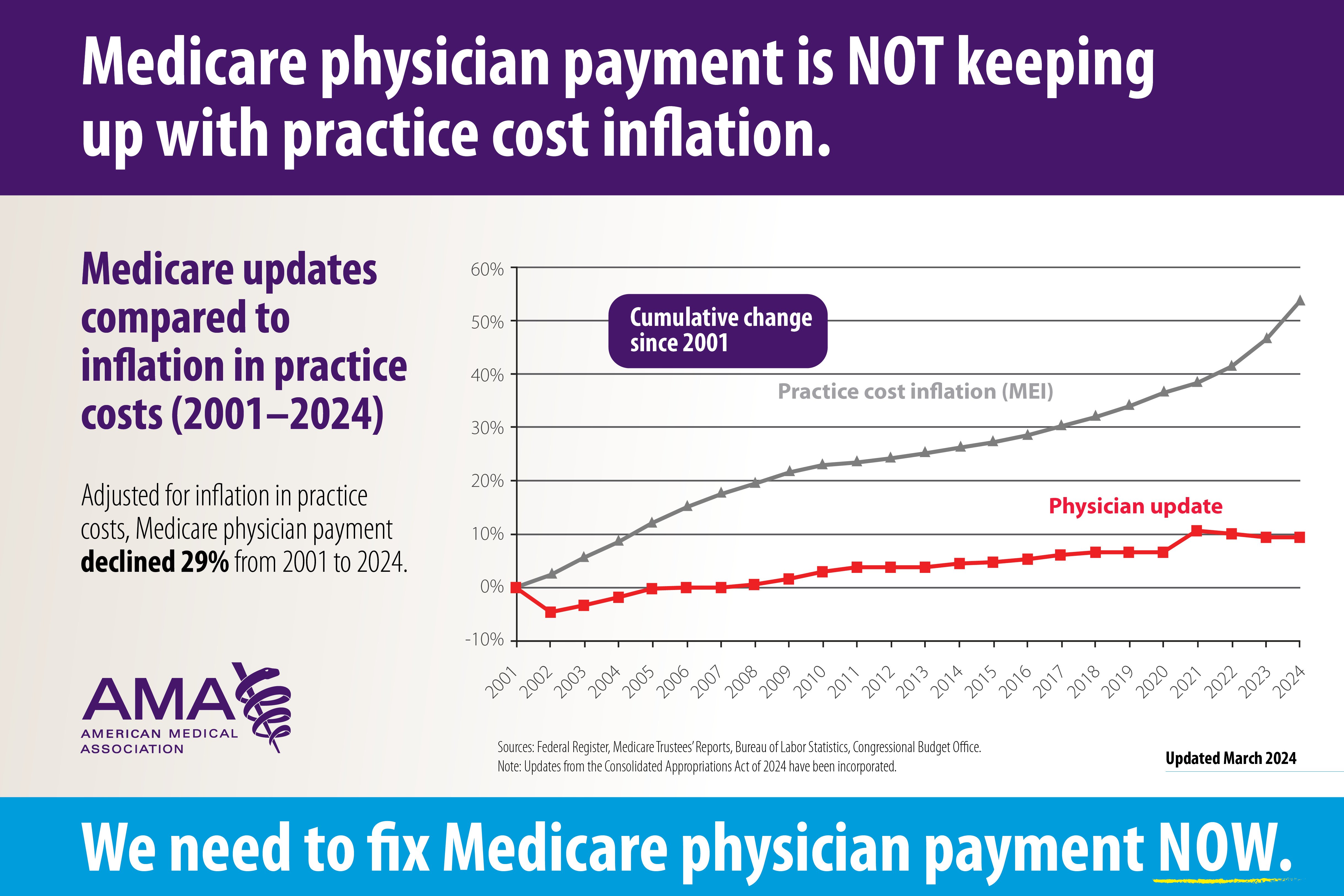
When adjusted for inflation in practice costs, Medicare physician pay declined (PDF) 29% from 2001 to 2024, or by 1.5% per year on average. According to the recently released 2024 Medicare Trustees Report, if physician payment does not change, access to Medicare-participating physicians will become a significant issue in the long term.
At the April 2024 meeting, MedPAC discussed two options to increase Medicare physician payment through annual, automatic updates. The first would update practice expense relative value units by the increase in the hospital market basket minus productivity. The second would increase Medicare physician payment by the Medicare Economic Index (MEI) minus one percentage point with a floor of half of MEI.
The letter outlines AMA concerns with the first approach, which would create disparities in payment based on specialty, risking worsening access problems for specialties with lower practice expenses, including psychiatrists and internal medicine physicians. Moreover, updating practice expense alone is insufficient.
Conversely, the AMA commended MedPAC for considering an alternative approach to update Medicare physician payment rates by MEI. However, the AMA firmly disagreed with MedPAC’s conclusion that because MEI minus one percentage point was historically adequate, it will sufficiently cover inflation in practice costs and ensure patients have access to care in the future. In addition, the AMA supported the continued need for Advanced Alternative Payment Model (APM) incentive payments to expand APM development and physician participation.
MedPAC’s June 2024 report to Congress will include an informational chapter discussing these options but will not contain any recommendations. The Commission will continue discussing this issue next year.
2022 Experience Report: MIPS bonuses increase, penalties hit small and rural practices
The Centers for Medicare & Medicaid Services (CMS) released the 2022 Quality Payment Program Experience Report (PDF) and summary (PDF) which provide an overview of physicians’ participation in the Merit-based Incentive Payment System (MIPS) and APMs in the 2022 performance period, which impacts payment in 2024. Approximately 87% of MIPS-eligible clinicians either avoided a penalty or earned a bonus for the 2022 performance year. However, the penalties continue to disproportionately impact small and rural practices.
Twenty-seven percent of small practices and 18% of rural practices were penalized. Almost 30% of solo practitioners received the maximum penalty of -9%. The specialties with the highest proportion of physicians receiving a penalty included anesthesiology and orthopedic surgery.
CMS attributed lower final scores overall to removal of quality measure bonus points, a change in the complex patient bonus methodology resulting in fewer clinicians being eligible for this bonus, the cost performance category being calculated for the first time since the 2019 performance period, and changes to performance category weights. In addition, the Extreme and Uncontrollable Circumstances hardship exception due to the COVID-19 public health emergency was not automatically applied in 2022; physicians had to apply for the hardship exception.
More articles in this issue
- May 17, 2024: Advocacy Update spotlight on the need for improved maternal health care
- May 17, 2024: National Advocacy Update
- May 17, 2024: State Advocacy Update