AMA summary: 2025 Medicare Physician Payment Schedule final rule
On Nov. 1, 2024, the Centers for Medicare & Medicaid Services (CMS) released the Calendar Year (CY) 2025 Revisions to Payment Policies under the Medicare Physician Payment Schedule (PFS) and Other Changes to Part B Payment and Coverage Policies final rule (PDF), and the AMA has developed a summary (PDF) of the 3,000-page regulation.
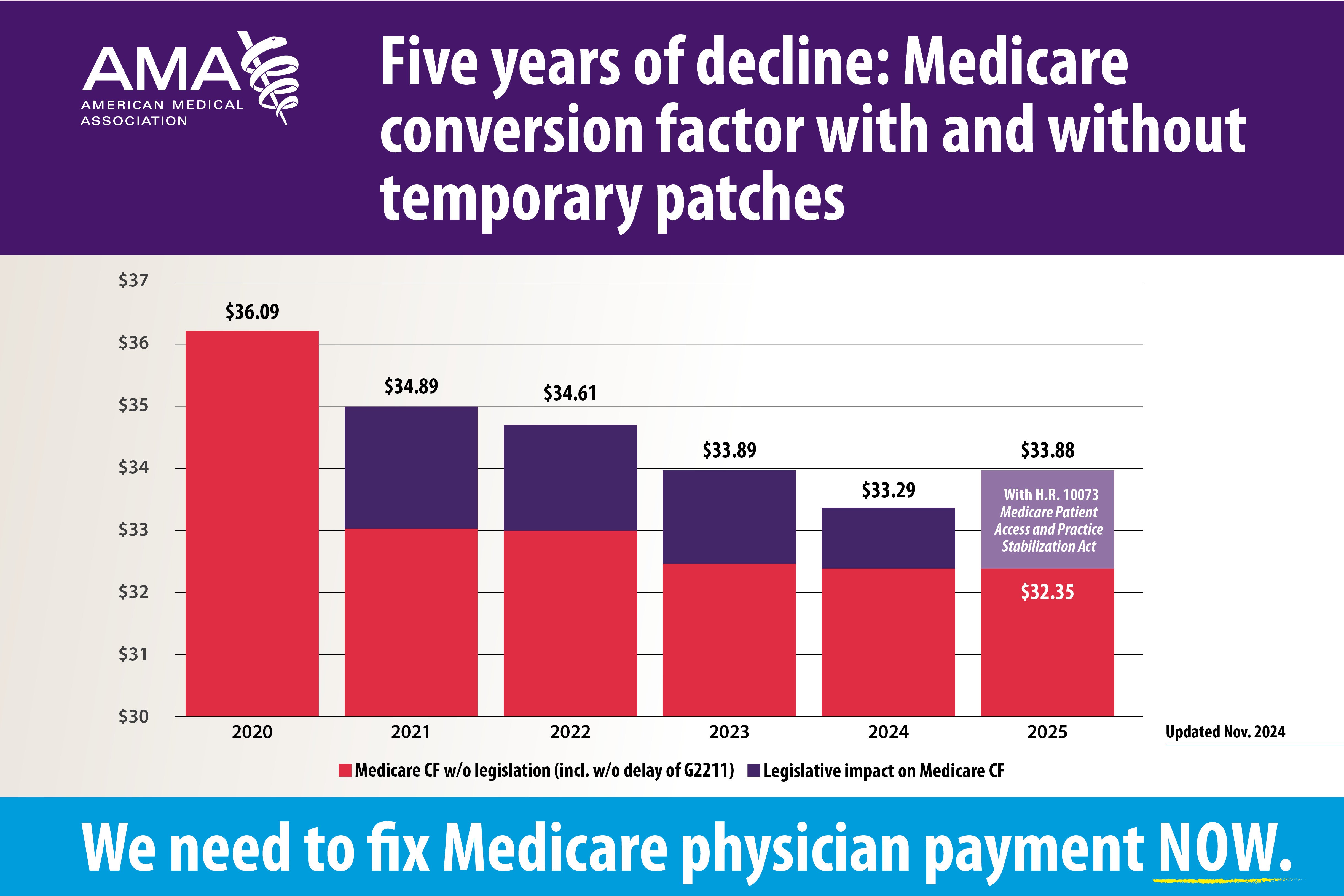
The 2025 Medicare conversion factor will decrease for the fifth straight year by approximately 2.83% from $33.2875 to $32.3465 (PDF). Similarly, the anesthesia conversion factor will be reduced from $20.7739 to $20.3178. Unfortunately, the 2025 cut coincides with ongoing growth in the cost to practice medicine as CMS has determined that the increase in the Medicare Economic Index (MEI) for 2025 is 3.5%. This is why the AMA and our partners in organized medicine are strongly supporting the bipartisan H.R. 10073, Medicare Patient Access and Practice Stabilization Act of 2024, which would stop the cut and increase physician payment rates by one-half of the MEI by applying a 12-month payment update of 4.73%.
For Medicare patients to retain access to telehealth services all over the country, not just in rural areas, and have them delivered to their home without having to go to a separate originating site, Congress must act before the end of 2024 to extend the COVID-era waivers of geographic and originating site restrictions under current law. The final rule includes policies that improve telehealth access in multiple ways, however. Most importantly, after nearly five years of AMA advocacy, CMS has finalized a permanent change to its definition of interactive telecommunications system to include audio-only services, not just audio-video. In a setback for medicine, however, CMS has finalized its decision to post the new CPT telemedicine evaluation and management (E/M) codes and relative values but, with one exception, not to adopt them for use in Medicare.
CMS will continue to delay implementation of the 2017-based MEI cost weights, pending the AMA’s Physician Practice Information (PPI) Survey. The AMA PPI Survey, a multi-year effort to measure physician practice costs and the direct patient care hours spent by physicians, concluded in August. The AMA will continue to work with Mathematica to analyze the data collected throughout 2024, intending to share with CMS in early 2025.
Finally, following ongoing advocacy by the AMA that CMS should not increase the Merit-based Incentive Payment System (MIPS) performance threshold due to significant disruptions caused by the COVID-19 pandemic and Change Healthcare cyberattack, CMS will maintain the threshold to avoid a MIPS penalty of up to 9% at 75 points for the CY 2025 performance year/2027 MIPS payment year. Research (PDF) continues to show that MIPS is unduly burdensome; disproportionately harmful to small, rural and independent practices; exacerbating health inequities; and divorced from meaningful clinical outcomes.
The AMA is strongly (PDF) urging Congress to make statutory changes to improve MIPS and address fundamental problems with the program by eliminating steep penalties that disproportionately hurt small and rural practices, prioritizing access to timely and actionable data, reducing burden, aligning MIPS with facility quality programs, and incentivizing the development and reporting of new clinically relevant quality and cost measures. For more details about the final rule, please review the AMA’s summary (PDF).
More articles in this issue
- Nov. 15, 2024: Advocacy Update spotlight on 2024 AMA Interim Meeting highlights
- Nov. 15, 2024: National Advocacy Update
- Nov. 15, 2024: State Advocacy Update