What’s at stake
The Medicare payment system is on an unsustainable path, threatening patients' access to physicians.
The system’s growing financial instability is due to a confluence of fiscal uncertainties physician practices face related to the pandemic, statutory payment cuts, lack of inflationary updates and significant administrative burdens.
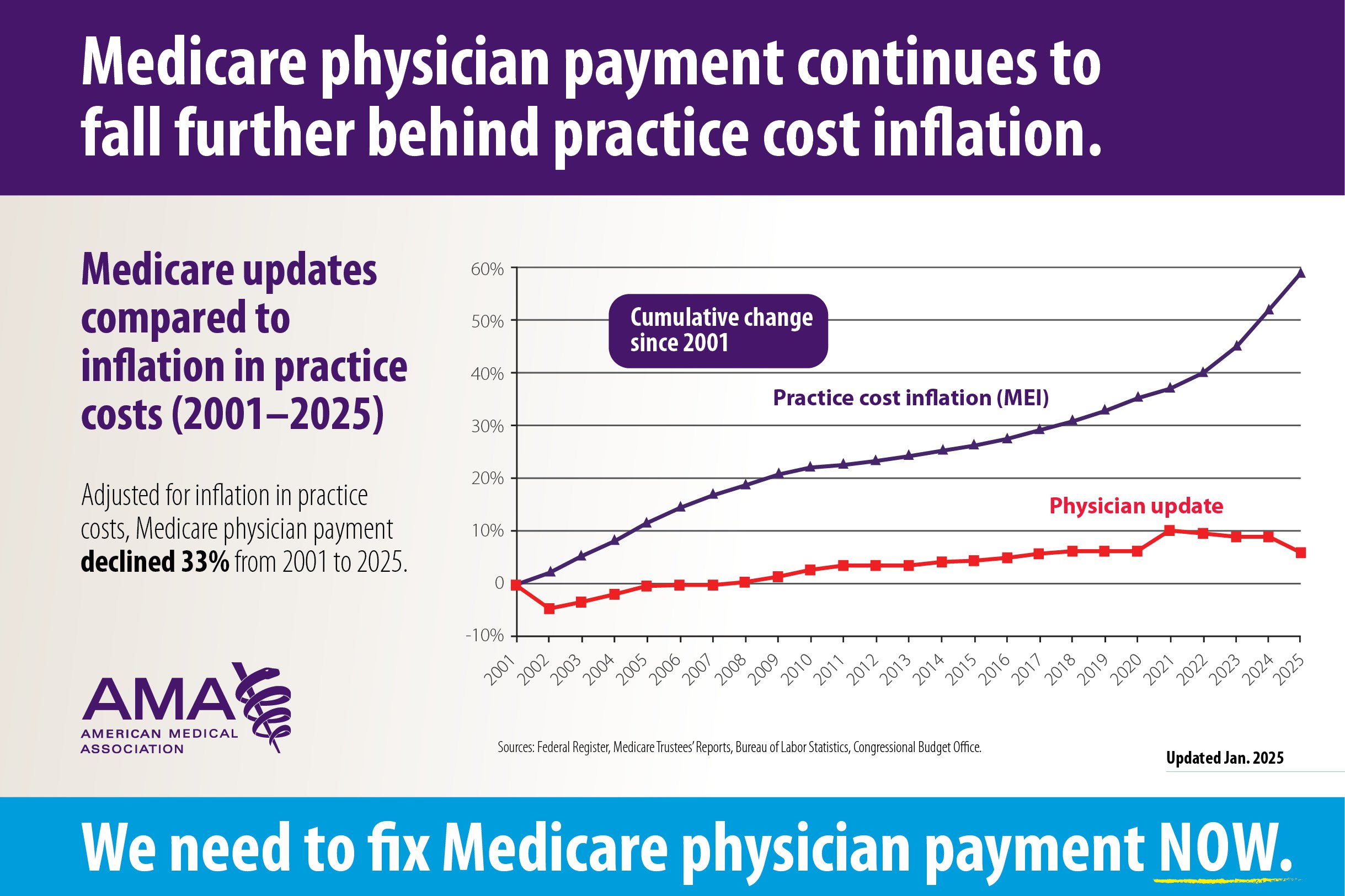
Medicare physician payment has effectively been cut 33%, adjusted for inflation, from 2001–2025. The Medicare physician payment system lacks an adequate annual physician payment update, unlike those that apply to other Medicare provider payments (PDF).
A continuing statutory freeze in annual Medicare physician payments is scheduled to last until 2026, when updates resume at a rate of 0.25% per year indefinitely, well below inflation rates.
A JAMA Health Forum study found that it costs an estimated $12,811 and more than 200 hours per physician, per year to comply with the Medicare Merit-Based Incentive Payment (MIPS) system and, to date, there have been very limited options for physicians to move towards value-based Medicare Advanced Alternative Payment Models (APM).
The discrepancy between what it costs to run a physician practice and actual payment combined with the administrative and financial burden of participating in Medicare is encouraging market consolidation and threatens to drive physicians out of rural and underserved areas.
The AMA’s position
Reforming Medicare physician payment means putting the patient back in the center of health care. That’s why it is a top priority of how the AMA is fighting for physicians, and why the AMA is working to block payment cuts, advocate for physicians and patients and build long-term solutions.
It is urgent that Congress work with the physician community to develop long-term solutions to the systematic problems with the Medicare physician payment system and preserve patient access.
Congress needs to establish a permanent, annual inflationary Medicare physician payment update that keeps up with the cost of practicing medicine and encourages practice innovation.
Budget-neutrality policies need to be revised to:
- Prevent erroneous utilization estimates from causing inappropriate cuts.
- Clarify the types of services that should and should not be subject to budget neutrality adjustments.
- Raise the projected expenditure threshold that triggers the budget neutrality adjustment, which has been in place since 1992.
The performance and reporting programs in Medicare’s MIPS are based on outdated legacy programs and the four components largely function independently and are noncohesive. They are burdensome and often lack clinical relevance. Policymakers should work with the physician community and other stakeholders to develop ways to reduce the administrative and financial burden of MIPS participation and revise reporting programs to ensure its clinical relevance to patient care.
AMA advocacy in action
The AMA has:
- Developed a set of principles (PDF) supported by more than 120 other medical societies to guide advocacy efforts on Medicare physician payment reform.
- Achieved consensus across medicine to pursue four pillars of Medicare payment reform:
- Establish an annual inflation-based payment update for Medicare physician payments.
- Revise policies and processes used to adjust payments to maintain budget neutrality.
- Simplify and improve the clinical relevancy reporting programs under the Merit-based Incentive Payment System.
- Extend policies that support practices wanting to transition to value-based payment systems.
The AMA is:
- Urging Congress to pass the Medicare Patient Access and Practice Stabilization Act (H.R. 879), which would prospectively cancel the 2.83% payment cut that went into effect on Jan. 1, while also providing a 2.0% payment update.
Advocacy resources
- Recently adopted AMA policy on Medicare payment.
- Chart: Medicare conversion factor with and without temporary patches (PDF).
- Chart: Medicare provider updates for 2025 (PDF).
- Chart: Medicare updates compared to inflation in practice costs (2001-2025) (PDF).
- Chart: Key measures of practice expense in the Medicare Economic Index (PDF).
- The principles: Characteristics of a rational Medicare physician payment system (PDF).
- Use the Physicians Grassroots Network to tell Congress to protect America’s Medicare patients.
- Learn about how you can take part in the fight to fix Medicare on behalf of your patients and practices at the AMA's Fix Medicare Now website.
- The AMA's Medicare Basics series provides an in-depth look at important elements of the Medicare physician payment system.
Learn more
Visit AMA Advocacy in Action to learn more about the advocacy priorities the AMA is actively working on.
Get involved
The AMA works to generate support for policies critical to the nation’s health care system—and we can’t do it without your help. Learn more about ways to get involved with AMA advocacy.