Medicare physician payment—often called Medicare reimbursement—must be tied to an inflation index called the Medicare Economic Index (MEI). As part of its campaign to fix the unsustainable Medicare pay system, the AMA has outlined in a quick, easily navigable fashion why this payment fix needs to happen now.
The AMA’s two-page explainer on the Medicare Economic Index (PDF) outlines how it incorporates these two categories reflecting the resources used in medical practices:
- Physician practice costs, which includes components for nonphysician compensation such as fringe benefits, medical supplies, professional liability insurance and other expenses. Each component is assigned a weight and various proxy indices are used to estimate price changes.
- Physician compensation, which reflects increases in general earnings and is currently proxied by changes in the wages and benefits of professional occupations in the U.S. from the Bureau of Labor Statistics. The change in the combined practice costs and physician compensation components of the MEI is then reduced by the 10-year average of economywide, multifactor productivity.
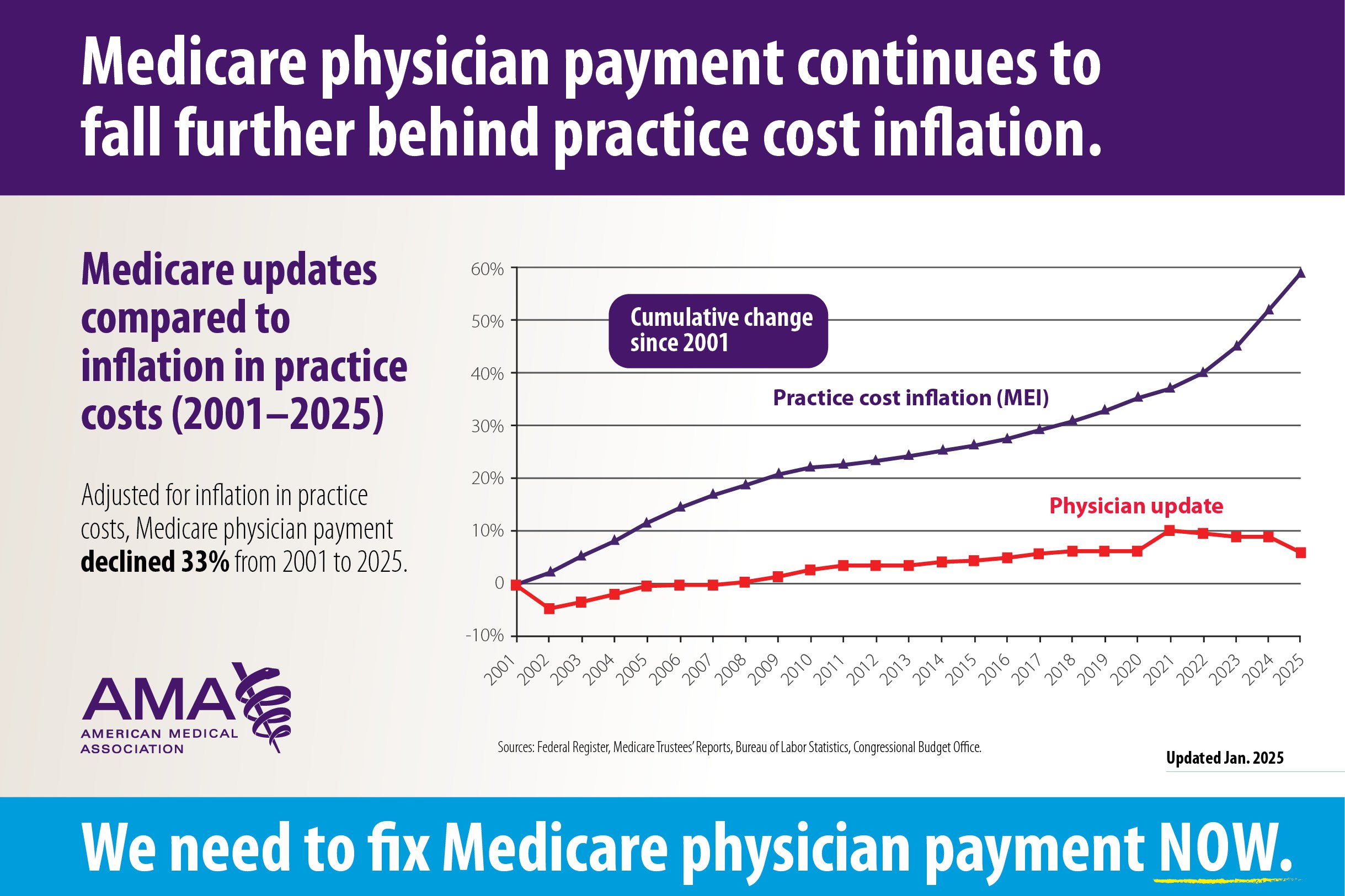
The big problem is that since 1992, the role of MEI in shaping Medicare physician payment has diminished dramatically, first under the sustainable-growth rate (SGR) and then under the Medicare Access and CHIP Reauthorization Act (MACRA) of 2015. Given those changes, it comes as no surprise that when adjusted for inflation, Medicare physician payment has effectively declined (PDF) 33% from 2001 to 2025.
Jason Goldman, MD, a Florida internist, is among the practicing physicians and AMA members who have taken time to share their firsthand perspectives on the impact of unsustainable Medicare physician payment in interviews with the AMA.
Dr. Goldman said Congress needs “to fix Medicare now, not just because physicians need to be paid fairly, but because the patients need their physicians. And if they do not fix Medicare, we will not have a health care system.”
The AMA is leading the charge to reform the Medicare payment system.
Long-term impact on care
Experts widely acknowledge that chronically inadequate Medicare payment rates will eventually take a toll on older adults’ access to high-quality care.
This was recognized again recently in the 2024 Medicare Trustees Report, which noted that “certain features of current law may result in some challenges for the Medicare program.” The payment system that MACRA put in place avoided significant short-range physician payments that the SGR system created; however, there are still payment concerns that future legislation needs to address.
“Physician payment update amounts … do not vary based on underlying economic conditions, nor are they expected to keep pace with the average rate of physician cost increases,” the report says. “These rate updates could be an issue in years when levels of inflations are high and would be problematic when the cumulative gap between the price updates and physician costs becomes large.”
The trustees wrote that “absent a change in the delivery system or level of update by subsequent legislation, the Trustees expect access to Medicare-participating physicians to become a significant issue in the long term.”
Meanwhile, the Medicare Payment Advisory Commission (MedPAC) voted in April to urge Congress to link Medicare payment updates for physician practices to the growth in the cost of providing care—a timely recommendation as lawmakers wrestle with how to handle yet another cut in physician pay.
Among the evidence MedPAC weighed was that physicians are experiencing a fifth consecutive year of payment cuts while medical inflation remains high. Physicians are abandoning private practice, and patients—especially in rural and underserved areas—face obstacles to accessing care. The recommendation came as Congress failed this spring to stop or reverse a 2.8% cut in Medicare payments for this year despite several proposals to do so.

At its meeting in April, MedPAC voted to recommend that Congress change the baseline increase to physician payment from 0.25%—or 0.75% if participating in an alternative payment model—under current law to a portion of MEI, such as MEI minus 1 percentage point, every year for the foreseeable future.
Emergency physician John Corker, MD, said in an interview with the AMA that “over about the last quarter-century, doctors’ offices and physician practices have been dying a slow death by a thousand paper cuts as it pertains to Medicare reimbursement.”
He noted that no other aspect of health care has experienced the pay cuts that physicians have experienced, noting that physician Medicare payment is the only one not tied to annual inflation adjustments. Hospitals and other health professionals see a Medicare rate change annually tied to inflation.
“Doctors are forced to make difficult decisions about what days they can be open, what staff that they can afford to pay, and as a result what services they can provide for their patients. And I think at the end of the day, it all comes back to access. If doctors can't keep their doors open and they can't have appropriate staff because of dwindling reimbursement rates for Medicare, patients can't access services from their doctors,” said Dr. Corker, a delegate for the Ohio State Medical Association in the AMA House of Delegates.
Physicians can take action now through the AMA’s Fix Medicare Now website to urge Congress to pass the Medicare Patient Access and Practice Stabilization Act (H.R. 879), which would replace the 2.8% cut for 2025 with a 2% Medicare reimbursement increase.
Catch up on Medicare’s basics
While the AMA is working relentlessly to build understanding on Capitol Hill about the unsustainable path the Medicare payment system is on, preventing further cuts means getting to the root causes of what’s wrong with Medicare physician payment.
That is why the AMA created the Medicare Basics series, which provides an in-depth look at important aspects of the Medicare physician payment system. With these six straightforward explainers, policymakers and physician advocates can learn about key elements of the payment system and why they are in need of reform.
Dive deeper to learn how Medicare pay cuts:
- Endanger physician practices.
- Threaten patients’ access to care.
- Especially affect rural America.
- Hit solo physician practices hard.
- Put even big medical groups at risk.
Visit AMA Advocacy in Action to find out what’s at stake in reforming Medicare payment and other advocacy priorities the AMA is actively working on.