As physicians everywhere struggle to overcome pandemic-related fiscal uncertainties and ever-increasing practice costs amid soaring inflation, we continue to be undercut by an unsustainable Medicare payment model that is bad for physicians, bad for patients, and bad for our health system.
Two alarming charts show the degree to which physicians are being squeezed by the current payment model, as Medicare physician payment has dropped by 22% adjusted for inflation between 2001 and 2021, according to an AMA analysis of Medicare trustees’ data.
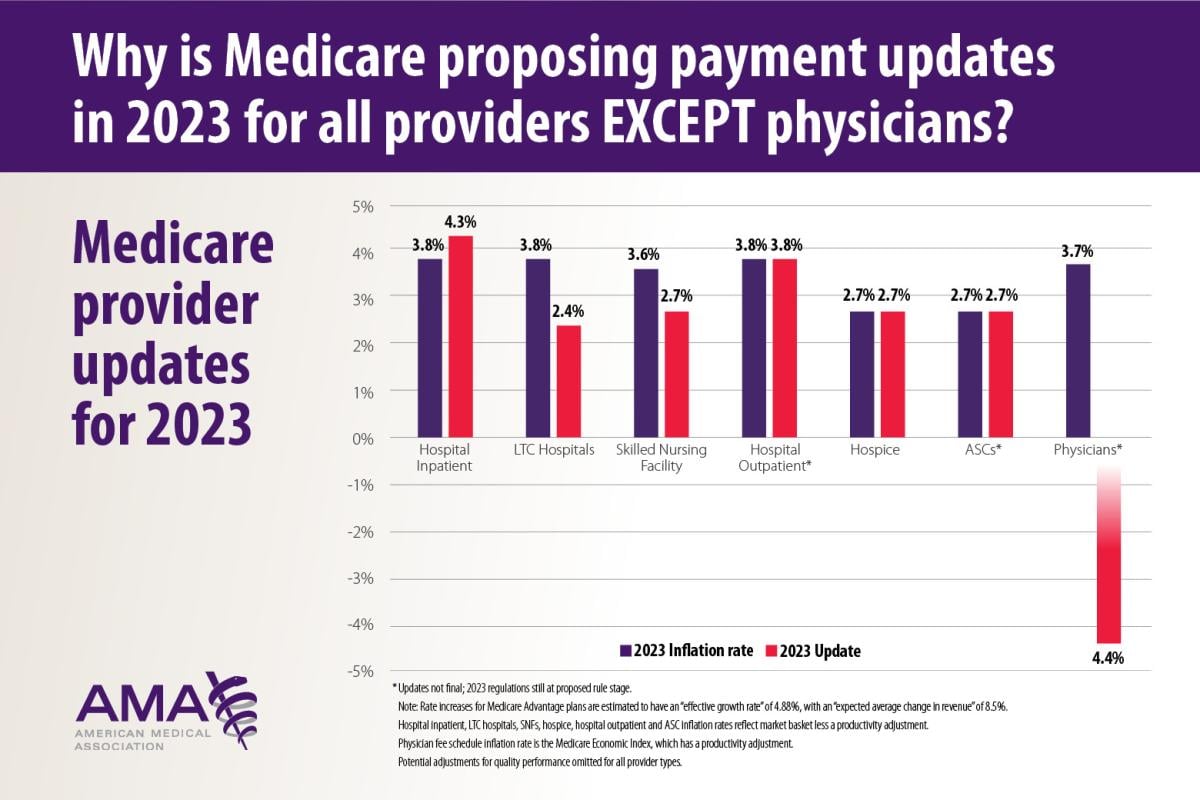
The news gets worse in 2023 as the Centers for Medicare & Medicaid Services (CMS) is proposing positive payment updates for hospitals, nursing facilities, hospice care, and ambulatory surgery centers—everyone except physicians, who are scheduled to get a 4.4% pay cut.
An irrational and unfair system
This is neither sustainable nor rational, and it is deeply unfair to physicians who are holding together a healthcare system stretched far too thin.
The Medicare physician payment system lacks an inflation-based annual update, in stark contrast to the automatic increases given to others who bill Medicare. Need more evidence? Spending per enrollee for other parts of Medicare jumped by between 3.6% and 42.1% over the last decade, even as spending on physician services per enrollee dropped by 1%.
Absent substantial legislative changes by Congress, circumstances stand to get even worse. A statutory freeze in annual Medicare physician payments is scheduled to continue until 2026, when updates resume at the anemic rate of 0.25% for an indefinite period.
That level of increase will hopelessly trail the inflation rate, even if inflation retreats dramatically from its current 40-year high. Even worse, budget-neutrality rules that penalize physicians for changes beyond their control will trigger further reductions in Medicare physician payments, beginning with a 4.42% cut on Jan. 1, 2023, unless Congress acts beforehand as it did last December.
Rebuild health care the right way
Reshaping the Medicare payment system to ensure financial stability and predictability, while safeguarding access to high-quality, value-based care, is a core element of the AMA Recovery Plan for America’s Physicians, along with fixing prior authorization, stopping inappropriate scope of practice expansions by non-physicians, continuing coverage of coordinated telehealth, and addressing the concerning rise in physician burnout. It’s time our nation supports doctors and removes obstacles that interfere with what drew us all to medicine in the first place: caring for patients.
This summer, the AMA released characteristics of a more rational Medicare payment system. This practical, commonsense approach to reform already has the support of more than 100 physician organizations.
Predictability is a key ingredient. Physicians need and deserve automatic, positive payment updates tied to practice costs they can rely upon, just like hospitals, skilled nursing facilities and others already have in place. Annual payment rate adjustments should be linked to a measure of practice cost inflation, such as the Medicare Economic Index.
We must also eliminate or replace budget neutrality measures that penalize physicians for conditions outside their control, and that fail to recognize the tremendous cost reductions that physician-led quality improvements have brought forth in other areas, such as reduced hospitalizations.
Rather than layering on burdensome reporting requirements for measures that seldom feel relevant, physicians also deserve access to timely, actionable data, and incentives tailored to the distinct characteristics of different specialties and practice settings.
While maintaining a financially viable fee-for-service model, we also need a diversity of voluntary alternatives that invest in practice transformation. Alternative payment models designed by physicians can remove barriers to the innovation required to address the chronic disease epidemic our nation faces.
Health equity focus
We must also approach payment reform with a focus on health equity. Physicians need support as we care for patients from historically marginalized communities, work to address social determinants of health and combat discriminatory practices in health care delivery. Quality and value measures should be risk-adjusted and reflect the ongoing contributions of physicians to dismantle health inequities.
Ensuring that payment reform and innovations equip physicians to reduce inequities, rather than penalizing that work, will improve not only our health care system but the health of our nation.
Physicians put their lives on the line responding to the COVID-19 pandemic. It’s time our nation supports us by helping to remove the most common obstacles we face, barriers that too often get in the away of caring for patients.
Patients deserve better and physicians deserve better. As we emerge from the worst phases of the COVID-19 pandemic and prepare to take on whatever health crises come next, it is essential that Congress put the Medicare payment system on a more sustainable path.